Author's details
- Dr. Khashau Eleburuike
- MBBS (Ilorin) MSc. Global Health Karolinska Institute.
- Resident doctor in family medicine in Northern Sweden.
Reviewer's details
- Dr Okoro Austin Chigozie
- MBBS, MWACS, MPH, FWACS.
- Consultant Obstetrician and Gynaecologist. Evercare Hospital. Lekki. Nigeria.

- Date Published: 2026-01-03
- Date Updated: 2025-04-29
Family Planning for Patients in Sub-Saharan Africa
Key Messages
- Contraception allows individuals and couples to plan when to have children, improving health and well-being.
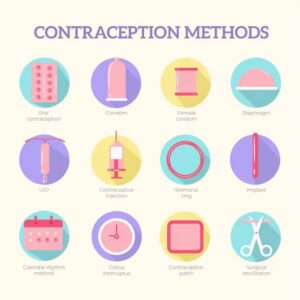
- There are various contraceptive methods, hormonal, IUDs, barrier, natural, and permanent. Each with different benefits and requirements.
- Choosing a contraceptive method depends on health, plans, access to care, and cultural beliefs.
- Myths about contraception are common, but most methods are safe, reversible, and do not cause infertility.
- Contraceptives are available at clinics, pharmacies, and through community health workers.
What is Contraception? Contraception, also known as family planning, refers to methods or devices used to prevent pregnancy. It allows individuals and couples to decide when or whether to have children, promoting healthier families and improving overall well-being.
There are many types of contraception, and each works in different ways to prevent pregnancy. It’s important to choose a method that suits your health, lifestyle, and future plans for having children.
Why is Contraception Important?
- Family Planning: Helps plan pregnancies and gives control over the number and timing of children.
- Prevention of Unintended Pregnancies: Reduces the risks associated with unplanned pregnancies, including maternal health complications.
- Health Benefits: Gives the body time to recover between pregnancies, reducing the risk of health problems for both the mother and baby.
- Prevention of Sexually Transmitted Infections (STIs): Some contraceptives, like condoms, help protect against STIs.
Common Types of Contraception Available in Sub-Saharan Africa
- Hormonal Methods:
Birth control pills: Pills that contain hormones (estrogen and progestin) to prevent ovulation. These need to be taken daily and are available in many healthcare facilities.
Injections (Depo-Provera): A hormone shot given every three months. This is popular in many regions because it is easy to use and doesn’t require daily attention.
Implants (e.g., Jadelle, Implanon): Small rods placed under the skin of the arm that release hormones and prevent pregnancy for 3-5 years. They are long-lasting and convenient.
- Intrauterine Devices (IUDs):
- Copper IUD: A small device placed inside the uterus that can prevent pregnancy for 5-10 years. It is non-hormonal and can be removed if pregnancy is desired.
- Hormonal IUD: Similar to the copper IUD but also releases hormones to prevent pregnancy. It can work for 3-5 years.
- Barrier Methods:
- Condoms (male and female): Condoms are widely available, affordable, and also help prevent the transmission of STIs, including HIV.
- Diaphragm: A shallow, dome-shaped cup inserted into the vagina before intercourse to block sperm. It is less common but available in some regions.
- Natural Methods:
- Fertility awareness methods: These involve tracking the menstrual cycle to avoid intercourse on the days when a woman is most fertile. This method requires careful monitoring and may be challenging for some.
- Withdrawal (pull-out method): A less reliable method where the male partner withdraws before ejaculation.
- Permanent Methods:
- Tubal ligation: A surgical procedure for women that permanently blocks the fallopian tubes. It is irreversible and recommended for those who do not want more children.
- Vasectomy: A permanent surgical procedure for men that cuts or blocks the tubes that carry sperm. It does not affect sexual performance.
Choosing a Contraceptive Method: The choice of contraception depends on several factors:
- Your health: Some methods may not be suitable for women with certain health conditions like high blood pressure or diabetes.
- Future pregnancy plans: If you plan to have children in the future, you may prefer temporary methods like pills, injections, or IUDs.
- Access to healthcare: Some methods, like implants or IUDs, require a healthcare provider for insertion or removal.
- Cultural and religious beliefs: In some communities, there may be cultural or religious considerations that affect family planning decisions. It is important to discuss contraception with your partner or a healthcare provider in a way that respects your beliefs.
Challenges in Sub-Saharan Africa:
- Access to Services: In rural areas, access to family planning services can be limited due to distance, cost, or lack of healthcare infrastructure. Many clinics offer family planning services, but women may need to travel long distances to reach them. Also lack of skilled manpower to carry out some of the procedures.
- Cultural Attitudes: There may be stigma or misinformation surrounding contraception. In some areas, contraception is mistakenly associated with infertility or promiscuity, which can discourage its use.
- Male Involvement: Engaging men in family planning discussions is crucial. Involving partners can improve acceptance and support for contraceptive use.
Myths and Misconceptions About Contraception
Myth: Contraception gives 100% protection from pregnancy.
Fact: It could reduce the risk for pregnancy. Some anticonceptions like hormonal IUD, copper IUD, Implanon has a protection from unwanted pregnancy compared to the natural cycles, condoms or withdrawal methods. See figure 1
Myth: IUD cannot be used by young women who have not given birth
Fact: As long as the IUD is inserted by a professionally competent midwife or medical doctor, the risk for complications is very low and IUD prevents unwanted pregnancies compared to pills that could be forgotten.
Myth: Breastfeeding is a form of anticonception.
Fact: Breastfeeding could prevent ovulation. It is a form of contraception called “Lactational Amenorrhoea Method” (LAM) which is a situation where the woman may not ovulate or see her menses. This is however not a reliable method except in the first 6 weeks after delivery if you exclusively breastfed your child. After 6 weeks, your ovulation can come at any time without you knowing.
Myth: Contraceptives cause infertility.
Fact: Most contraceptive methods are reversible and do not affect long-term fertility.
Myth: Hormonal contraceptives cause cancer.
Fact: Some forms of contraception like the combined pills may protect against certain cancers like ovarian cancer, endometrial cancer, bowel cancer. There can be a little increased risk of getting breast cancer in some pills and the hormonal IUD. However, the risk is relatively low among young women.
Myth: Those whose female relatives have had an hormone sensitive cancer cannot use hormonal anticonceptions.
Fact: Having a female relative with breast cancer does not increase your risk when using hormonal anticonceptions except if you have had a previous hormone sensitive cancer.
Myth: Condoms reduce sexual pleasure.
Fact: While some people may experience a difference, condoms are an important method for preventing both pregnancy and STIs.
Where to Get Contraceptives
Contraceptives are available in various places across Sub-Saharan Africa:
- Health centers and clinics: Most government and private clinics offer family planning services, often at no or low cost.
- Community health workers: In some regions, trained community health workers provide contraceptives and advice, especially in rural areas.
- Pharmacies: Some contraceptives, like condoms and pills, can be purchased over-the-counter without a prescription.
Contraception empowers women and couples to make informed choices about their reproductive health. While access to contraception varies across Sub-Saharan Africa, it is crucial to seek reliable information and services from healthcare providers. Family planning improves health outcomes, promotes economic well-being, and supports the development of healthier families.
If you need advice on which contraceptive method is best for you, talk to your healthcare provider or visit your nearest clinic.
- Sedgh G, Hussain R. Reasons for contraceptive nonuse among women having unmet need for contraception in developing countries. Studies in family planning. 2014 Jun;45(2):151-69.
- Sedgh G, Ashford LS, Hussain R. Unmet need for contraception in developing countries: examining women’s reasons for not using a method.
- Darroch JE, Singh S. Trends in contraceptive need and use in developing countries in 2003, 2008, and 2012: an analysis of national surveys. The Lancet. 2013 May 18;381(9879):1756-62.
- Frye CA. An overview of oral contraceptives: mechanism of action and clinical use. Neurology. 2006 Mar 28;66(66_suppl_3):S29-36.
